The new year is typically a time to reflect on the past 12 months and refresh our focus for the future. The last two years have been fraught with changes and challenges particularly for clinicians, and the start of 2022 has been no different.
COVID-19 has substantially diverted our attention and delayed progress in planning for the rest of the year. However, as leaders, it’s essential to take time, re-focus, and set the stage for what comes next.
Dr. Randy Pilgrim, SCP Health’s Chief Enterprise Medical Officer, offers six suggestions on strategic areas that will require focus during and after the pandemic.
Health Care Industry Change
Change has been an ever-present reality, increasingly pervading the entirety of health care. Innovation and transformative change will continue to be central themes moving forward. COVID-19 further catalyzed the need for more investment in domains such as analytics, telehealth, and post-acute care.
Driving forces include
- Effective access to care for target populations;
- Duration and scope of clinician accountability (e.g., acute care only, +30 days, + 90 days);
- Payment models (e.g., BPCI-A, ACO, FFS, etc.);
- Quality measurements, including reporting and payment.
Health care industry change is likely to pivot around key considerations like these, which drive patient care outcomes and health care economics. Clinicians must expect change, learn to manage it, and when necessary, drive it.
Evolution of Practice Models
Future practice models will diversify current clinical responsibilities, especially as value-based care and extensions of care “outside the four walls” of traditional practices become more common. Such diversification increasingly involves accountability for post-acute care, telehealth, and employee health programs. To be sustainable, diversified practice models must be supported by well-aligned reimbursement and compensation models.
A McKinsey report found that practice diversification can help organizations strategically protect and evolve core businesses if appropriately managed.
“Health systems that expand their ambulatory footprint, for example, not only gain new revenue streams but also may increase patient inflow to their acute care services,” the report said.
This diversification also presents an opportunity for clinicians to gain additional professional skills and reduce certain practice risks – for example, by becoming proficient in providing telemedicine care as an adjunct to in-person clinical care.
New Methods of Care Delivery
Digital transformation will be an increasing influence for new models of care. The report, “Digital Transformation in Healthcare in 2021: 7 Key Trends,” by Digital Authority Partners, a digital transformation leadership organization, listed the following areas impacting health care today:
- The rise of on-demand health care;
- The importance of big data in health care;
- Treating patients and training physicians with virtual reality;
- Growth of wearable medical devices;
- Predictive health care;
- Artificial intelligence;
- Addressing fragmentation in electronic health records through the use of blockchain technology.
Increasingly, emerging health care transformations like value-based care, improving health equity, and the use of data-driven decision support will require empowerment by technology and adoption by clinicians. It’s vital to lead, manage, and develop competencies accordingly.
Transformative Leadership
With so many issues and so much change, clinical leadership has never been more essential than it is now. Leaders must be planning for the future – after the storm – even if it’s not time to take action yet.
Clinical leaders help teams navigate change through influencing, motivating, and empowering people. They improve processes, cut out noise and distractions and focus the team on what matters. Well-executed leadership is not only effective, it can be transformative.
In his MLC21 medical leadership conference presentation, “Leading Transformation: What’s New? What’s Next?” Dr. Pilgrim listed several areas for clinical leaders to emphasize and implement:
- Communicate changes clearly. Refer directly to your group’s culture and patient-centered mission;
- Define and share an end goal;
- Establish a specific group to lead change;
- Foster a sense of urgency, balanced with appropriate patience;
- Encourage participation. Celebrate short-term accomplishments.
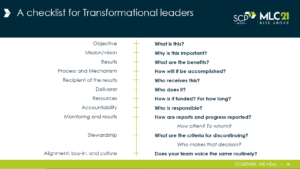
Transformation often happens best when it occurs internally, led by frontline staff. Dr. Pilgrim also emphasized the need for collaboration and positive culture re-affirmation, proposing that leaders use the following guide to communicate transformation.
Clinician Resiliency
Before the pandemic, the health care industry already had significant demands. COVID-19 has amplified and exacerbated those demands. Issues such as burnout, exhaustion, and staffing shortages have now become a routine part of health care delivery, rather than occasional setbacks.
For years, clinicians have been intentional about continuous clinical study to keep their clinical knowledge current. Now, clinicians must use a similar discipline to create an intentional plan that nurtures personal and professional resilience. Doing so enhances professional effectiveness, prevents burnout, and increases clinician and patient satisfaction.
Keeping the ‘Human’ in Health Care
Bureaucracy, technology, performance expectations, and increasing demands all challenge the human aspect of health care. But true healing requires the “bright light” of human-to-human compassion. Effective resiliency and mission-driven professionalism provides the fuel; the human touch turns that into healing.
Despite many pressures otherwise, this involves far more than improving patient experience scores. This is the essence of our profession – the patient-by-patient of genuine empathy and caring. In that respect, a good question (and constant reminder) is, “How have I been a ‘human’ to my team and to my patients today? And did I let them be a ‘human’ to me?”
SCP Health’s Mission in 2022 and Beyond
Using emergency medicine and hospital medicine as our foundation, SCP Health seeks to impact the entire continuum of care in the communities we serve.
Innovation and transformation are essential to streamlining clinicians’ work as we optimize systems, improve patient outcomes, reduce errors, and lower costs.
While the ways we do that are expanding beyond our traditional EM and HM foundations, our mission remains the same: deliver high-quality, patient-centered clinical care, every time.
Contact the SCP Health team to learn how we can help your organization succeed in providing the utmost innovative, transformative care.


