A Universal Challenge Requires Innovative Approaches
Health care is experiencing nearly universal reductions in revenue and unprecedented pressures on cost, which continuously challenge our status quo. At the same time – and more than ever – patients need better access to high-quality, cost-effective care and a more rewarding experience of their care. Fundamentally, hospitals and health systems must consider two things to achieve better outcomes at a sustainable cost: (1) deploying innovative services and (2) improving the impact of existing services.
Frequently, the emergency department is overlooked and underutilized in service of those objectives. Transformation requires a different view of current services, especially obligatory services with a high fixed cost like the emergency department.
Emergency Medicine: Looking Back
Since the specialty was established four decades ago, emergency medicine has matured substantially. We have a well-respected core mission – treating the acutely sick and injured – and have become a significant gateway to the entire hospital and health system. We have earned the trust of medical staff and community physicians, who increasingly rely on the ED as a diagnostic, stabilization, and treatment center for complex patients1.
However, while health systems and payors seek effective solutions for addressing the sickest and costliest patients, the ED is often bypassed. An episode of care in the ED is expensive when considered in isolation, but amazingly, opportunities to leverage that cost – even when the patient is right in front of us – are not frequently contemplated. We provide excellent care, and we point patients in the right direction when they are discharged. However, after their ED visit, patients often struggle with access to primary care, ineffective transitions of care, an inability to effectively navigate the health care system, and difficulty understanding their plan of care. All of this leads to suboptimal outcomes, poor engagement, and higher overall costs. Even when post-acute “solutions” are attempted, they are often disconnected and fragmented, and accountabilities are not aligned.
A ubiquitous issue in health care often repeats itself right under our watch. We have an opportunity to lead and an obligation to respond.
Emergency Medicine: Looking Forward
In the US, emergency departments are routinely visited by a remarkable proportion of the most medically intense and costliest patient populations. Up to 57% of patients in an average ED have been classified as “intermediate or complex conditions” (including chronic conditions like CHF, COPD, and diabetic complications, or acute conditions like abdominal pain, chest pain, and pneumonia)2.
Data are becoming more compelling each year, fueled by an increasingly aging population that has an even greater burden of comorbidities. Our experience in COVID-19 showed that even during the pandemic, these clinically intense populations consistently accessed emergency departments. As we recover from the pandemic, these patterns continue.
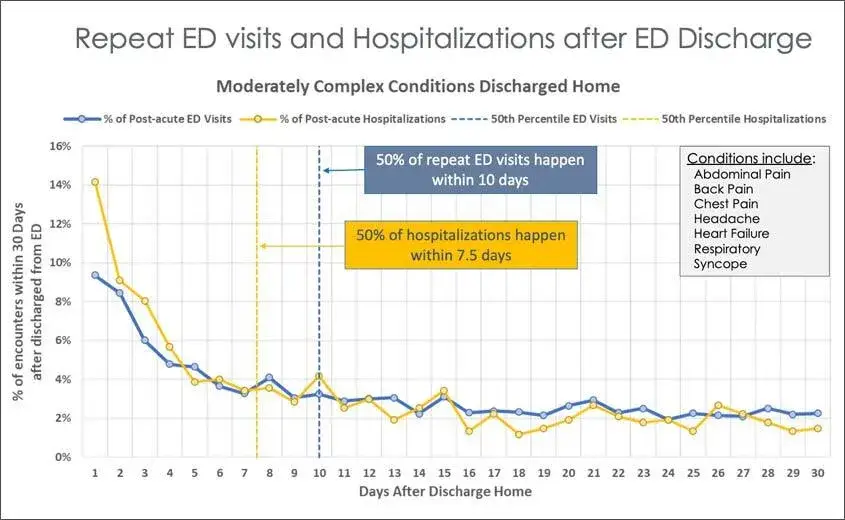
More than two-thirds of these moderately complex patients are discharged home into the same health care system that was unable to prevent many ED visits in the first place. Data from SCP’s enterprise data warehouse (hundreds of EDs) shows that when repeat ED visits happen for these populations, half occur within the first 10 days. Similarly, for hospitalizations that occur after an initial ED visit, half of those occur in the first 7.5 days.
Transformation in the Golden Window: “Care in the Gap”
The data are compelling. There is a golden window after an initial ED visit for key populations, during which there are potentially preventable repeat ED visits (which are costly) and potentially preventable hospitalizations (10 times more costly). Some ED re-visits and hospitalizations are necessary, but as we know from clinical practice, many are avoidable. Preventing expensive and avoidable visits requires interventions in the “Gap”.
The “Gap” is the space between the initial ED visit and either improvement in the patient’s condition or meaningful integration with longitudinal care (primary care physician, etc.). This involves:
- effective compliance with follow-up instructions, including medications;
- meaningful connection to primary care;
- effective navigation of the health care system, and
- clinical stabilization.
Point solutions and patient engagement strategies have been attempted by numerous stakeholders with modest success at best (case management, disease-specific management, social work, insurance company call centers, etc.). Many are not connected with the ED that provided the emergency care in the first place. Most address a small subset of this larger population. Many solutions are unscalable, which threatens sustainability. Most have difficulty meaningfully engaging patients. On balance, there are ineffective efforts to consistently address key populations, even when those patients routinely obtain acute, unscheduled care (such as an ED visit). Hence, our piece of the “universal challenge.”
The 7–10-day period after an initial ED visit is a golden window. Typically, patients are not entirely better, are adjusting to a different plan of care, and are not yet able to access primary care. Many do not (or cannot) follow the prescribed plan of care or don’t understand what they should do. As Figure 1 notes, over half of the repeat ED visits and subsequent hospitalizations happen during this period – some of which are avoidable.
Avoiding preventable ED visits and hospitalizations requires a different approach. The ED is well-positioned to impact care transformation with straightforward approaches and modest incremental investments. Most of these involve post-ED care before the patient is meaningfully connected with primary care. This is “Care in the Gap.”
The ED has an opportunity to make a big impact if we extend our reach. But we won’t get different outcomes if we do the same things we’re doing today. To make a change, we must extend our reach outside the four walls. We must respect everything that’s working in emergency care and not place unworkable demands on clinicians who are already challenged with clinical efficiencies. But something needs to change.
Transforming Care After COVID
At SCP Health, we are working intensively to address these challenges. Building on our long-term strategy, we are launching from an excellent clinical foundation and now, seeking to address the full continuum of care in the communities we serve. We don’t intend to deliver primary care long-term, but we fully intend to address “gaps” in care with effective and meaningful bridges. In doing so, we will improve outcomes, reduce costs, help hospitals grow, and continue our innovative pathway.
Part 1 is a brief summary of the core elements of the bridge: supporting care and delivering care. In brief, we either “Support” care in the gap, or we “Deliver” care in the gap.
1. Support care in the gap:
Rather than providing new clinical care, we assist patients in effective transitions of care and basic, non-clinical navigation of the health care system. Often, non-clinical interventions have the greatest overall impact, even for moderately complex conditions. Examples:
a. Patient navigators (telephonic, non-clinical interventions):
- Find primary care physician for patients without one
- Obtain a timely appointment
- Ensure that the patient went to the appointment
- Ensure that the patient follows their discharge instructions
- Encourage filling and taking prescriptions as ordered
- Full transition to primary care (or appropriate specialist) as soon as possible
- Escalate to nurse or physician if needed
b. Nurse follow-up (telephonic, nursing interventions):
- Answer additional questions about instructions for care and transitions
- Escalate to NP/PA or physician as required
- Full transition to primary care (or appropriate specialist) as soon as possible
2. Deliver care in the gap:
This option connects patients with a post-acute clinician who addresses care in the “Gap” with a new clinical encounter. A physician, NP, or PA provides one of several options as appropriate, including:
- Telemedicine visit
- Home visit
- Nurse or independent practitioner
- SNF encounter
- Return to ED if needed
These low acuity visits are designed to deliver continuity of care, address straightforward clinical issues, and prevent unnecessary escalation and bounce-backs. Part 2 of this series will articulate the solutions in more detail.
Summary
Because the ED sits at the very nexus of the inpatient and outpatient worlds, there is a considerable opportunity to impact patient care during the most immediate timeframes after discharge from the ED. Especially for high-focus populations, we have an opportunity to impact clinical quality, improve patients’ experience of care, create better outcomes, and reduce overall cost.
SCP is invested in innovative solutions that build on our excellent clinical foundations. Addressing post-acute “Care in the Gap” will extend our team’s reach while connecting it with our clinician’s original visit. At SCP, we have both an opportunity and an obligation to continuously improve as we continue to build excellent clinical systems of care.
References:
1 Gonzalez Morganti, Kristy, Sebastian Bauhoff, Janice C. Blanchard, Mahshid Abir, Neema Iyer, Alexandria Smith, Joseph Vesely, Edward N. Okeke, and Arthur L. Kellermann, The Evolving Role of Emergency Departments in the United States, Santa Monica, Calif.: RAND Corporation, RR-280-ACEP, 2013. As of July 12, 2021: https://www.rand.org/pubs/research_reports/RR280.html
2 Smulowitz PB, Honigman L, Landon BE. A novel approach to identifying targets for cost reduction in the emergency department. Ann Emerg Med. 2013;61(3):293-300. doi:10.1016/j.annemergmed.2012.05.042






