It has been just over one year since COVID-19 began to sweep across the world and since President Trump declared a public health emergency on March 13, 2020.
Following that announcement, the healthcare system has been riding a tumultuous rollercoaster. Each twist and turn has left our nation’s hospitals, providers, and patients searching for a way out of the pandemic wilderness.
Despite the challenges, the pandemic has also revealed meaningful opportunities for hospitals and health systems to strengthen their roots, reset expectations, and establish new pathways to improve patient care and overcome financial hurdles.
On March 10, two SCP Health executives, Lisa Fry, Chief Growth Officer, and Joseph Rose, MD, Senior Vice President, Group Medical Officer, conducted a webinar with Modern Healthcare— COVID’s Call to Action: Reset for Success in 2021—looking back at the past 12 months and ahead to the remainder of 2021 and beyond while discussing lessons the healthcare industry has learned and what the future may hold.
We pulled information and comments from the webinar to compose a series of posts touching on three key learnings: improving patient access and loyalty, how healthcare executives can better support clinicians, and changes in consumer behavior due to the pandemic.
In this post, we discuss:
- The Pandemic’s Effect on Society
- Effects on Hospitalized Patients and Clinicians
- Steps Hospitals Took to Provide Access and Improve Loyalty
- Telehealth’s Role in Restoring Patient Access and Loyalty
- What the Future Looks Like for Patient Access and Loyalty
The Pandemic’s Effect on Society
News of the pandemic was a harbinger of drastic change. Schools closed for months, and some are still closed. Theaters, restaurants, and businesses closed. Millions lost their jobs, leaving a financial impact the world hasn’t seen since World War II, according to The World Bank.
Normal activities ground to a halt as people sequestered in their homes, for fear of falling victim to the virus were they to leave.
Recalling his personal experience, Dr. Rose said, “Living next door to my mother- and father-in-law, because they were in their late 70s, they decided to be careful and cautious. … I hadn’t seen them in the last year unless they were on their back porch waving from a distance with a mask on.”
Truly, the effect of the pandemic on our society is unlike anything we have experienced in our lifetime or will likely ever experience again.
Effects on Hospitalized Patients and Clinicians
Undoubtedly, hospitalized patients were the worst victims of the pandemic due to the need for separation from families, high morbidity, and a mortality rate that left some hospitals with little, if any, space to house the deceased’s bodies.
Friends and family members of COVID patients suffered greatly as well, agonizing over the inability to be with their loved ones, especially during the last moments of their lives. It is a tragedy of immense proportions by anyone’s estimation.
“If you have loved ones with COVID in the hospital … one out of three of those folks in the early days weren’t surviving,” Dr. Rose said. “You knew that they were basically going to pass alone, and that was a big deal for us as patients [and] as citizens honestly.
The pandemic’s effect on physicians and other clinical staff also took a severe physical and emotional toll, from securing the necessary PPE (and improvising when enough couldn’t be found) to concern for their families and addressing volume surges.
“Patient volumes increased to 120 percent — physicians went from seeing 18 to 20 patients per day to 30 patients per day, and from 15 or 16 shifts per month to 26,” Dr. Rose said. “People’s emotions were getting fragile.”
Add to that the stress of talking with families of severely ill COVID patients.
“I can still remember talking with the husband of a 42-year-old teacher who was just admitted,” he said. (She later died). “That wasn’t a once-a-month kind of thing but once per day. … There was a price to pay there, and we paid it in hospitals.”
Steps Hospitals Took to Provide Access and Rebuild Trust
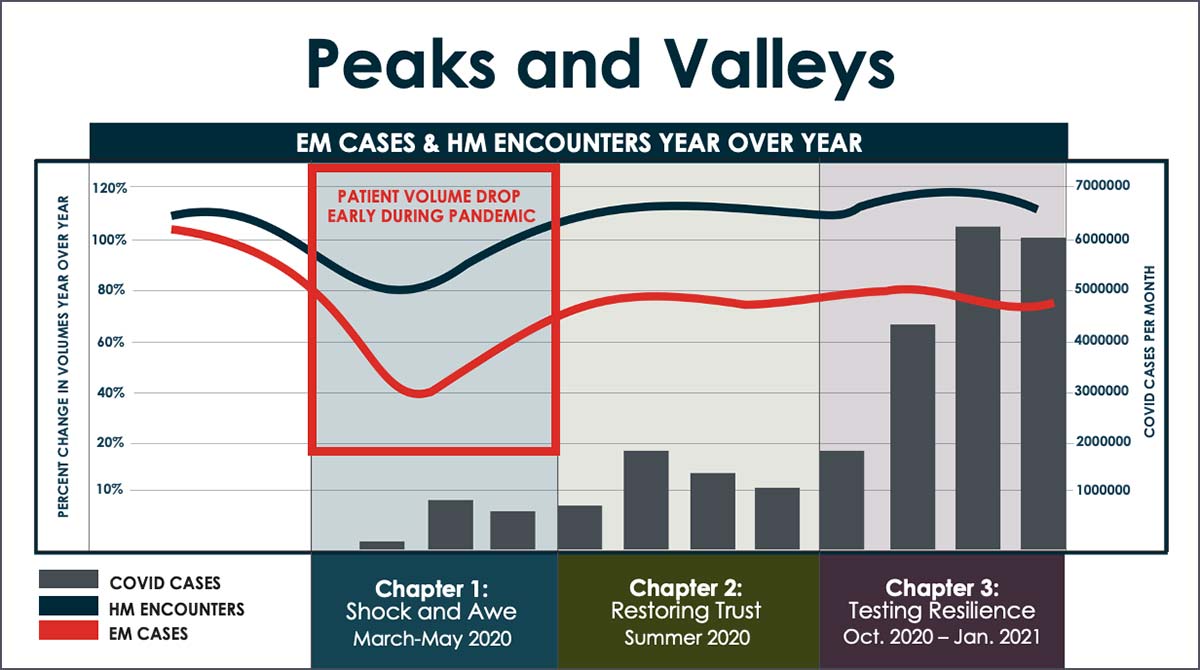
In a poll, webinar attendees ranked increasing patient volume and regaining trust as top priorities—not surprising, considering that early on, emergency department visits dropped dramatically due to fear of exposure, and elective surgeries were either postponed or canceled.
The unanticipated adverse effect on revenue that resulted from the decline forced hospitals and systems to engage in efforts to restore volume and rebuild trust in healthcare services’ safety.
Remarking on these efforts, Fry said, “We focused on PSA campaigns to educate patients that it was safer to seek care if you really needed it. We didn’t want folks having heart attacks at home. So, we focused on that and on rescheduling elective surgeries and created models for how to prioritize who got back on the schedule first and second and third.”
As hospitals began to grasp COVID’s ferocity in fuller measure, treatment protocols like drive-through testing and improving emergency room safety were implemented to increase patient volumes and restore loyalty.
“Volumes did start to recover in the emergency room but were still 20 percent below what they normally were,” Dr. Rose said, adding that hospital medicine volumes returned to 100 percent.
“Unfortunately, it was with COVID patients, and those patients are certainly a lot sicker, and a lot more difficult to deal with. So, some stressors did start to come on board,” he said. “But, again, at least we started to have some treatments we could offer as far as patients go.”
Telehealth’s Role in Restoring Patient Access and Loyalty
Telehealth and telemedicine played an increasingly vital role in improving patient access and loyalty.
“Early on in the pandemic, out of necessity, we set up zoom triage stations and tents in parking lots outside of EDs, but by April, CMS had put the waivers in place, and those had gone into effect,” Fry said. “[W]e focused on building out additional capabilities in telehealth, both inside the walls of our facilities for folks who were there but needed some separation, as well as in the outpatient environment.”
This chart shows a meteoric rise in overall telehealth-enabled visits as a result of the pandemic.

What the Future Looks Like for Patient Access and Loyalty
What does the future look like where patient access and loyalty are concerned?
“We are in a pivotal moment,” Fry stressed. “We’re not fully out of the woods yet … but we could make decisions and take actions today that could become critical foundations and building blocks for your post-pandemic position within your market and your community, with your clinicians and staff, and with your patients.”
Fry urged hospitals and systems to focus on positioning for the future.
“We all have some work to do to refocus on rebuilding volumes. Will you build them in the same service lines you had in 2019, or will you look to invest in different places? How best can we support our community’s needs? What role should health systems play in that and perhaps in maybe different ways than we have in the past?”
She cited educating the public on vaccine information and distribution as one short-term example.
“[I]nvesting in getting that right today can pay dividends in terms of your patient loyalty and community stature for the future,” she added.
At the end of the webinar, Fry said that while access to care was significantly disrupted in 2020, a silver lining is that the medical community has found new ways to give people access and restore loyalty, with trends toward outpatient care and telehealth.
“Telehealth and technology, in general, allows us to segment and customize messages much more effectively than when you did a billboard that may not appeal to a certain audience. Better apps to customize messages to the community with whatever messages make the most sense to them. The pandemic has shown us that one size doesn’t fit all.”
Regarding patients’ and the public’s view of the future (which he thinks is optimistic thanks to the vaccines), Dr. Rose drew on a recent experience with his mother- and father-in-law.
“Last week, about three weeks after they had been vaccinated and my wife and I had been vaccinated, we all sat down and had lunch together,” he shared. “And for the first time in literally a year, I shook the hand of my father-in-law … and hugged my mother-in-law, and it was incredible. It was huge.”
View SCP Health’s webinar COVID’s Call to Action: Reset for Success in 2021 on-demand, now, for more tips and resources for positioning your health system to succeed in a post-pandemic environment.
Other Resources:


