Understanding the scope of clinician well-being
A few years ago, my wife and I drove through the night, from Arizona back to our home in Colorado. The next afternoon she was stumbling through her day and blurted out, “I feel terrible after being up all night.”
My response? “Welcome to how I’ve felt about every fourth day for over 30 years.”
From medical school rotations to last year, ages 20 to 54, I walked the hallways of hospitals at all hours of the day and night, and I can tell you from firsthand experience – your clinicians are almost all unwell; they were unwell before you hired them.
The state of clinician well-being
Among the public, there is often a general feeling that clinicians who are burned out have been practicing too long, or are at least firmly into the middle years of their career. However, the data does not reflect that assumption.
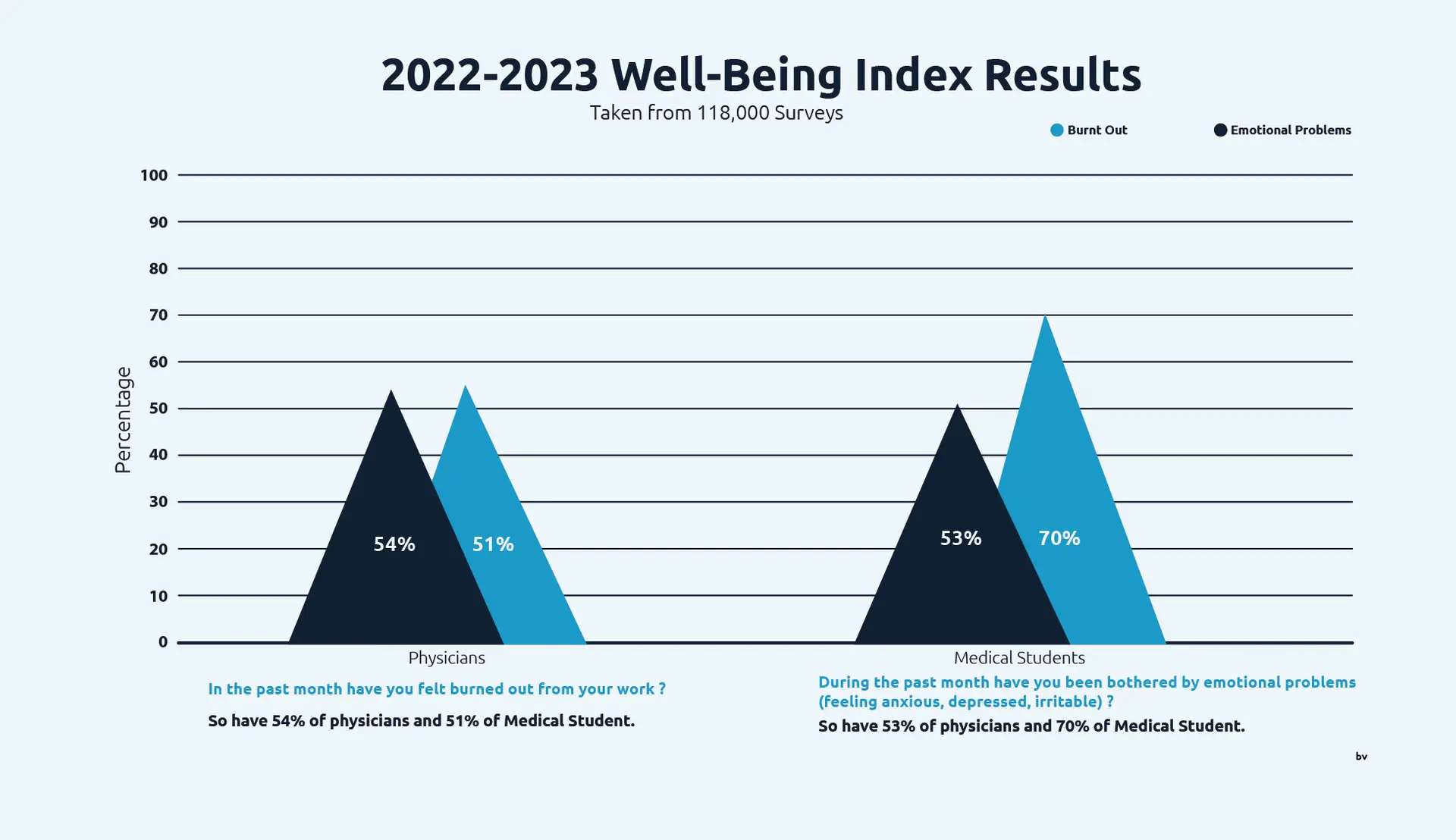
The 2022-2023 Well-Being Index surveyed well over 100,000 heath care workers – with many being physicians and medical students. Their results were startling.
When asked, “In the past month, have you felt burned out from your work?” 54% of physicians and 51% of medical students said yes.
In response to the question, “During the past month have you been bothered by emotional problems, feeling anxious, depressed, irritable?” 53% of physicians and 70% of medical students once again answered in the affirmative.
Another study, one that looked at clinician burnout by career stage, had similar findings:
- Early career (0-10 years) clinicians had a 50% burnout rate.
- Mid-career (11-20 years) clinicians had a 54% burnout rate.
- Late career (>21 years) had a 40% burnout rate.
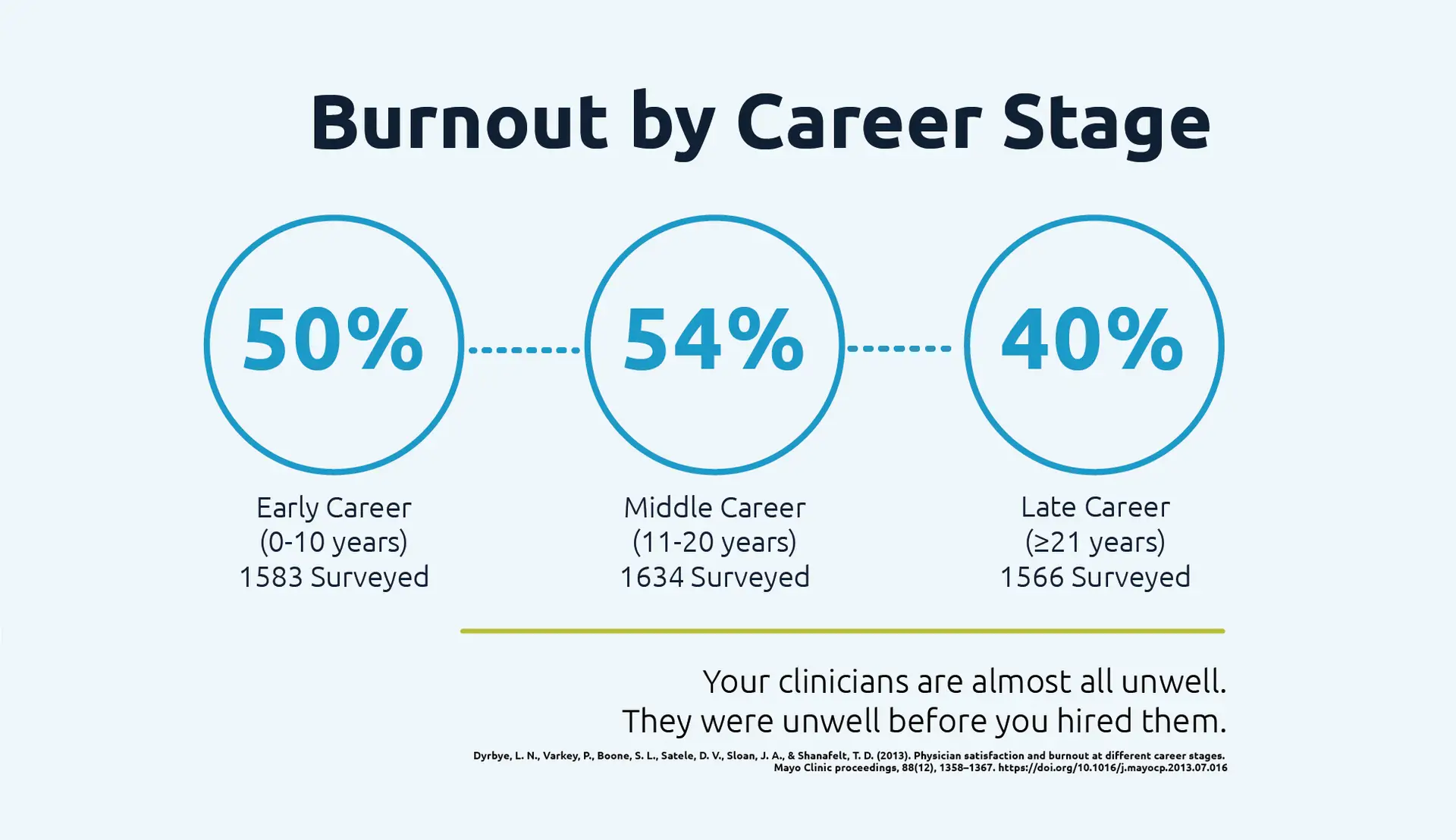
No matter where a clinician is in their career, from med school to the late stages, there is a better than even chance they are burned out.
The costs of clinician burnout
In addition to being concerned about the cost of burnout for clinicians themselves, from a human standpoint, there are other impacts of clinician burnout that must be considered.
Clinician turnover
Clinicians who are burned out are more likely to leave. A 2021 study of clinicians found that burned out clinicians were twice as likely to want to reduce their hours and nearly three times as likely as the not burned out peers to say they planned to leave their position in the next two years.
A 2022 study of a 500-clinician health care system looked at the financial costs of turnover and estimated the impact at $4.9 million for that system. Turnover is typically the sole metric used to determine the costs of burnout. There is no question that the clinicians who left due to burnout are costing a lot.
But what if those turnover costs are less than 1/3 of the total red ink? What if they are less than 25%?
The ones who stay
The cost of the clinicians who are burned out and left is far outweighed by the ones who haven’t yet left. Burnout erodes the mental health of clinicians, impairing their ability to care for patients. This can lead to decreased fulfillment and productivity and increased medical error and malpractice lawsuits.
That same 2022 study looked at the productivity impact of clinician burnout and did a comprehensive wellness assessment, comparing RVUs of clinicians who qualified as burned out to the scores of those who did not. The findings estimated that burned out clinicians still practicing in this 500-clinician system were annually costing up to $18.5 million by reduced productivity.
Health systems can’t afford to ignore clinician well-being
Clinicians are unwell – at every career stage and in every specialty. The impacts of clinician burnout are felt throughout our health care system – by our patients, clinicians, hospitals, and communities. This problem is not new and it’s not going away. It will not improve without direct action on the part of hospital and health system leaders.
We can not afford to ignore clinician well-being.
Learn more about the economic impact of clinician well-being.




