This is the second of a two-part series on the changes taking place in 2024 to the Bundled Payments for Care Improvement Advanced (BPCI-A) Medicare payment plan. The first post covered what BPCI-A is and what will change starting January 2024. In this post, I discuss the program’s importance to physicians, benefits to patients, and what is required to run a successful BPCI-A program.
BPCI-A is essentially moving all of us into the realm of population health management, and it is making us much more responsible for costs.
As providers, we have been very sheltered from costs in the past. Very appropriately, we concerned ourselves with providing the best possible care regardless of price tag. Those times are now changing. We are still being asked to provide the highest quality care. However, now we are being asked to make sure that any intervention we make that costs more than expected truly elevates quality and provides better care. If that intervention does not improve quality or outcome, then it is not worth the expense, which is a key consideration as we are held financially responsible for overall cost.
Why Should Providers Care About BPCI-A?
There are three reasons why providers and clinical leadership should care about BPCI-A:
First: 90-Day Outcomes: The New Standard
Like it or not, 90-day outcomes are now a standard by which all providers will be measured. In addition to quality measures, we are now also measured on all costs that occur during hospitalization and for 90 days after. When we sign the discharge order, our names are programmatically attached to all costs that occur for the next 90 days.
Second: Medicare Is Just the Beginning
Right now, BPCI-A is relegated to Medicare, but we believe commercial insurance plans will likely follow suit. A large commercial payer in Louisiana is now starting a similar program with emergency departments where those facilities are now responsible for all costs 30 days after the emergency room visit. SCP leadership believes this type of bundled payment system is ultimately where most payment models will go.
Third: Reimbursements are Changing
Take a moment to look at the graph below. Your salary (labor costs) is represented by the green line at the top, but the blue line is how much money we’re getting reimbursed by payers. It’s clear that these trends are not sustainable.
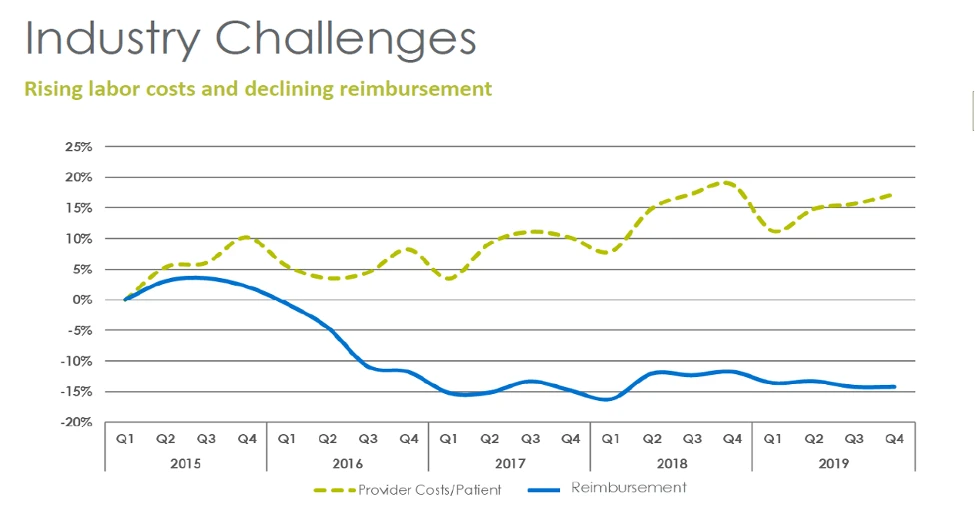
We’ve always known that reimbursements from self-pay and Medicaid payers are well below our accrued costs. Most facilities almost break even on costs with traditional Medicare. Traditionally commercial insurance has covered our costs of care for these other payer populations; however commercial insurance rates are now dropping to a fraction of what they used to be. Given these times of decreasing reimbursements, succeeding at BPCI-A has become a necessity to remain financially viable. We must learn to be successful based on Medicare reimbursement levels.
Does BPCI-A Really Benefit Patients?
The chief concern for clinicians is that their patients receive great care and great clinical outcomes. As clinicians, we often feel torn in two different directions when we’re told we need to care about costs as well.
However, Medicare has structured BPCI-A in such way that it’s a Win-Win situation both for cost and for patient outcomes.
We all know that care outside of the hospital could be better. Any provider on call in the last 2 weeks knows that at least 50% of admissions could have been avoided if patients had seen their PCP the week before or if they would have had better follow-up care after a recent admission. There are too many cracks in our outpatient network. Because of this, a lot of patient harm and financial waste occurs in the 90 days post hospital discharge.
When we improve care after discharge and decrease patient harm, money is saved. Quality of life goes up. Medicare spend goes down. We all win. The only way to be successful in this program financially is to make your patient’s total care after hospitalization of higher value and quality by decreasing SNF length of stay, emergency room utilization, readmission rates, and mortality rates. With BPCI-A, everybody wins.
BPCI-A Levers for Success
We have 4 main levers to pull to help us achieve success in this program. We’ll discuss each of them below.
- Next Site of Care: Optimize utilization of an appropriate care setting. Post-Acute Care has the potential to be very expensive. As you’ll see below, LTACs, SNFs, and inpatient rehabs have huge costs associated with them. Do all the patients we send to these facilities truly need this level of care?
- Performance Networks: We will now be responsible for every dollar spent by SNFs and every readmission from those SNFs. Creating networks that only the highest quality and lowest cost facilities can be members of forces a competition that ultimately benefits our patients by providing high quality and high value care.
- SNF Length of Stay: Medicare believes that for most bundles in BPCI-A, a patient should have to stay no more than 14-22 days. Why, then, do some SNFs hold on to patients for 6 weeks? This wide variability in length of stay with minimal, if any, improvement in outcomes needs to be addressed.
- Readmissions: Reduce avoidable readmissions through proactive patient care management.
More on Next Site of Care. Why is it Important?
This table below shows what each Next Site of Care costs both Medicare and Patients.
No matter what, it is essential to remember that as a clinician, you are responsible for the patient first and cost second. The goal is not to limit services for limiting services sake.
If a patient would benefit from expensive care, then give them expensive care. This is not rationing. If they need IRF or an LTAC, please send them there. If they do not, however, limit the unnecessary utilization of resources that, in the end, will not contribute to a patient’s outcome or quality of care.
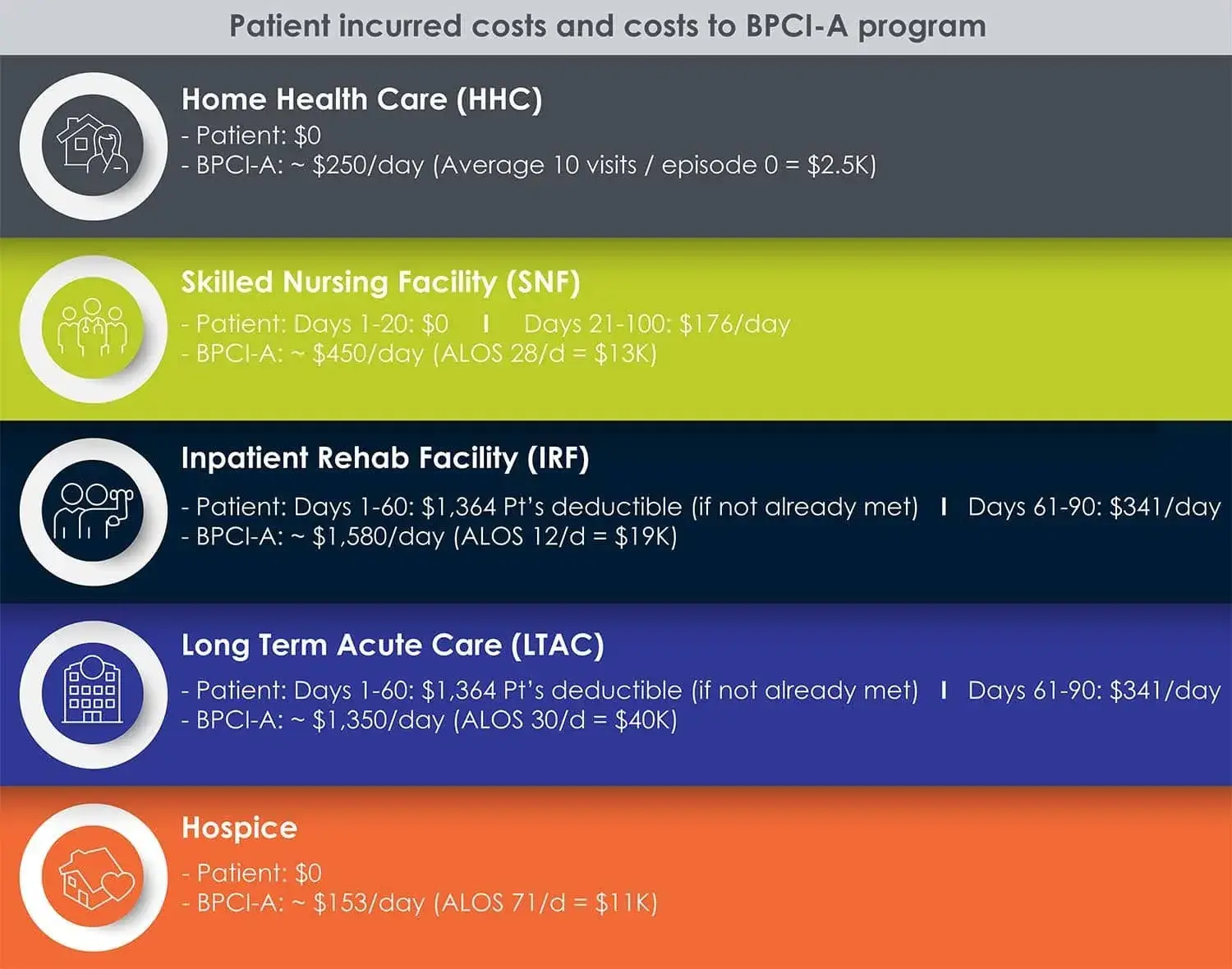
Home Health Care (HHC)
As you can see, home health care as a rule of thumb is $2,500. That’s inexpensive compared to some of the other options.
Skilled Nursing Facilities (SNF)
With an average price tag of $13,000, obviously this is more expensive than going home. However, it is typically much less expensive than an Inpatient Rehab Facility if the SNF has an appropriate length of stay (21 days or less). If necessary, it is our job to be sure we’re recommending facilities with low readmissions and appropriate lengths of stay.
Inpatient Rehabilitation Facilities (IRF)
Inpatient rehab is roughly $20,000. This is tailored for patients who have had strokes or other conditions that necessitate intensive therapy in two of three therapy lines that include PT, OT and or Speech. This is not meant or designed for people who are simply weak from a UTI or a pneumonia. To send this type of patient here is adding on an additional $8,000 on average to their cost of care when their needs could have easily been met at the local SNF. You have not increased value or quality, but you have increased cost when you do this.
Long-term Acute Care (LTAC)
LTACs cost on average $40,000. These facilities are meant for very sick individuals that require long term acute hospital care. An example of the level of patient who would require this level of intervention is a patient who is intubated, has a tracheotomy, has a PEG tube for enteral feedings, and who won’t be off the ventilator for another few weeks. It’s not meant for simple IV antibiotics or wound care which could be provided at home or in a SNF for less than half the cost. LTACs are used on average <1% of the time nationally, so if your utilization rate is higher, then look very closely to be sure you’re not overutilizing these expensive facilities at no benefit to your patients.
Hospice
Lastly, we have hospice, at an average of $11,000. If you know your patient will not survive more than a few months—no matter what interventions are done—then it’s our (clinician’s) job to have that discussion with the patient. They can choose to stay home to enjoy their remaining time and hopefully avoid frequent re-admissions along with the associated trauma. Ultimately, it’s our patient’s choice, but we must be proactive and thorough in discussing all the options. This is a key part of delivering highly compassionate and exceptional quality care.
Why Not Home?
“Why not home?” is an initiative in next-site of-care that we feel strongly about. This is the question we should ask ourselves about every patient when we’re considering discharge. There are some patients where the answer is an obvious “no”. However, for many, the choice to send home or to institutionalize is not as obvious. Given the benefits in both cost and quality of life, and given the massive resources home health now offers, it must be considered strongly.
Benefits of Sending Patients Home
As you can see from this list, sending patients home when appropriate and feasible offers many benefits:
- Faster recovery, better long-term outcomes, and happier, healthier, more secure patients
- Lowers the risk of complications (less exposure to resistant infections).
- Patients are less likely to develop delirium. Early dementia patients put into institutions are more likely to sundown in the unfamiliar surroundings. Sedating medications may follow to control behavior, and as we know, falls and fractures could then result.
- Institutionalization seems like the safer option at first glance — but when you think about it, is it really? Be sure.
- Better patient satisfaction
- More private, quiet, and familiar environments.
- Better access to friends and family.
- (Example: My father was quite upset when he was hospitalized for a DVT during his fight with cancer. He had little time left. He wanted to be home.).
- More judicious use of Medicare benefit
- Save SNF days for when they’re needed.
- Keeping a patient home another year or two before institutionalization is for many good for body, mind, soul, and the longevity of Medicare.
Post-Acute Care Safety Net
As you can see from the above, there is a lot of financial waste in our post-acute space. We have SNFs that hold on to patients for 4-6 weeks instead of the 2-3 recommended by CMS. We have poor patient follow up post-discharge. Readmissions are way too high. Lastly, we have huge gaps in communication between the myriad of providers who lay hands on our patients after leaving the hospital. CMS is now saying, “enough!” Too many patients are falling through the cracks. Too much money is being wasted. Either we fix it, or we pay for it.
In this country, our “post-acute care safety net” is not nearly strong enough. We must make it stronger.
SCP’s Four-Pronged Post-Acute Care Strategy
At SCP Health, our goal is to offer a best-in-class post-acute care safety net for every patient we treat. To that end, we have developed a four-pronged system designed to take care of the patient when they leave the hospital.
Post-Acute Care Solutions (PACS)
We offer to put a nurse practitioner into any nursing home around our sites.
It won’t cost nursing homes a penny, and they know those patients will be seen by a qualified provider every day. Expanding telehealth into this realm for nights, weekends, and holidays is also something that we are actively looking into. We want to increase the level of care in our SNFs.
Patient Engagement Solutions
Our Patient Engagement Solutions are a suite of patient- and community-centered services that we’re currently expanding throughout the country. One of the services offers virtual case managers who call every patient when they leave the hospital to ask questions like:
- Do you have your medications?
- Do you have your follow-up appointment?
- Are you feeling okay?
If the patient isn’t feeling well, the case manager gets them an appointment, either via telemedicine or at a local PCP’s office. We also have virtual nurses (registered and licensed) who can step in to help when needed.
Post-Acute Care Field Representatives
We have individuals who follow the patients to the nursing home to ensure they get the care that they need and plan for discharge at the appropriate time.
Population Health Data Base Development: mySCP Care App
You can’t engage in population health without good data. Acquiring data from multiple sources from hospital to post-discharge is not easy. We’ve developed the mySCP Care app. It is both a mobile and web-based tool where patients are entered into the system during hospitalization. They are then followed by our post-acute field representatives who then log in their various locations and outcomes as they progress from one stage of care to another. With this data, we can better aim our efforts where needed most.
Wouldn’t it be nice if we could someday add a patient portal to this app so they could reach out to us when necessary? Yes, we’re actively thinking on how we might make our system better.
Conclusion
In this two-part series, we first defined what BPCI-A is and outlined its purpose. We then looked at why this program is important to you (the provider), and we showed how BPCI-A could benefit your patients. Lastly, we gave you a glimpse of the future SCP Health is envisioning for this program and how it will transform the face of medical care for the better.
Medicare’s goal is to improve quality, reduce financial waste, and thus raise the level of value that we are getting for the money we spend. Of course, much of the program’s success relies on our willingness to aggressively implement the ideas above moving forward.






