
Patient Loyalty Through the Emergency Department
Home » Patient Loyalty Through the Emergency Department
Patient Loyalty Through the Emergency Department
Home » Patient Loyalty Through the Emergency Department

Home » Patient Loyalty Through the Emergency Department
Home » Patient Loyalty Through the Emergency Department

Patient satisfaction is currently treated as one proxy for the quality of care a patient receives. Admittedly subjective, satisfaction survey scores are nonetheless put to all kinds of concrete purposes, from reimbursement to performance pay. While satisfaction scores undoubtedly help gauge the experience of a single episode of care, they ultimately fall short of a larger, more important goal: to get patients to see the health system and its providers in a spirit of long-term partnership and collaboration— not just from scheduling to billing, but from year to year and decade to decade.
Instead of focusing on episodic patient satisfaction, in other words, the way to create real value in today’s industry is to earn consumers’ loyalty.
In this white paper, we help provider organizations understand the benefits of expanding their vision of the patient experience from a singular or episodic view to a lifetime view of healthcare and partnership. We identify the larger context making this shift necessary and then analyze three domains of change that will help health systems earn patients’ trust beyond a single episode of care.
When health systems fully grasp the difference between loyalty and satisfaction, they stand to solve a host of seemingly unrelated challenges, from the rise of self-pay to the proliferation of online feedback (via Facebook and Twitter as well as online ratings sites) to the decrease in patient volume. The cultural shift necessary to elicit true loyalty from patients may even help stem clinician burnout: instead of transactional care aimed at scoring high on a single survey, clinicians would be rewarded for treating every patient like a valued, long-term partner.
In short, although the larger context here is one of financial strain and increased competition, the solution may ultimately result in a model of care in which providers feel authentic and effective— and patients feel they have truly received personalized care.

Since 2012, a portion of a health system’s revenue has been tied to its scores on the Hospital Consumer Assessment of Healthcare Providers and Systems Survey (HCAHPS). Value-based Purchasing (VBP) policies have also established financial incentives for excellent performance on satisfaction measures. While such programs have pushed health systems to devote more attention to patient satisfaction, they may have made that focus too narrow. Resetting sights on patient commitment would better serve health systems’ need for financial sustainability and their mission to deliver the highest quality care.
The average American now spends $10,348 per year on healthcare. When a health system earns a patient’s loyalty, not just their intermittent satisfaction, it stands to make a significant, compounding difference to its bottom line.
Most important, the engagement and partnership bound up in the notion of loyalty stands to improve that patient’s life. After all, the point of providing the “highest quality care” is long-term patient health— something that can’t be achieved (or measured) with a piecemeal, episodic approach.
On the patient side, rising out-of-pocket costs for healthcare have converted them into more careful, and warier, consumers: they’re approaching healthcare services with greater cost consciousness; consulting consumer information sites intended to help them make more informed choices; and paying much closer attention to health system mentions on social media and other informal registers of patient experience.
With access to insurance expanding dramatically over the last decade, insurance companies have shifted more of the costs of care to patients and their families (partly through higher premiums but more significantly through the creation of high-deductible health plans).
Not only is the payment experience something that’s been shown to affect satisfaction, it’s likely to impact loyalty as well. Think about it: What are the two products of a health system visit that tend to persist long after the patient returns home? 1) A health status that’s altered, hopefully for the better—and 2) the bill.
“Ours is quickly becoming an experience economy,” observes Joseph Fifer, President and CEO of the Healthcare Financial Management Association.
The new-to-healthcare concept of the “experience economy” provides a useful framework for thinking about patient commitment. This framework explains consumer choices not as cold, objective calculations but rather as decision-making processes involving emotion, memory, and trust. And while Fifer is referring mainly to patients’ financial experience in a healthcare setting, providers should remember that patients’ experiences affect their trust and their engagement, which in turn impact health outcomes.
We recommend starting the shift to loyalty in what may seem like an unlikely place: the emergency department (ED).
Why shouldn’t loyalty-minded health systems start instead with orthopedics, or some other unit where many of the services are elective and most are high-revenue—meaning that matters like reputation, proof of strong outcomes, and brand are already on their radar?
Because the emergency department is considered the “front door of the hospital” for a reason.
While most people think of the ED as the epitome of episodic care, it is also the first—and most memorable—experience many patients will have with a given health system. That opportunity should be understood as a crucial job interview for providers, one where anticipating needs, reaching beyond the four walls of the hospital, and using data to enhance patient experience stand to make the greatest impression.
The ED is more than just the health system’s front door, though. It is also its public face.
EDs serve the full community, accounting for a sizable portion of health system admissions and providing a vast range of care in an unpredictable, often stressful setting. Those very challenges combine to create a prime area of opportunity: because the ED is a place where patient expectations are often low, and changes for the better will be both immediately noticeable and more appreciated than ones made in more controlled areas of healthcare. That appreciation can be amplified when it appears online, either on social media or in dedicated hospital comparison sites.
If you Google any hospital, roughly eight out of every 10 reviews will be about the ED. A recent study in the Annals of Emergency Medicine establishes the most effective levers for addressing that feedback.
The 2018 study compared over 100,000 online Yelp.com reviews of emergency departments and urgent care centers, focusing especially on 1-star and 5-star reviews of the two settings. The authors found certain themes to be common to 1-star reviews of both EDs and urgent care centers, and certain themes to be different; they observed other commonalities and differences for the 5-star category.
Their conclusions provide helpful guidance for health systems looking to foster patient commitment from the ED:

“Themes associated with 5-star reviews among EDs and urgent care centers were similar for comfort, professionalism, facilities, pediatric care, and staff interactions”; those that were unique to stellar reviews of EDs included bedside manner, care for family members, and access.
The levers: reinforcing the positive effect of bedside manner with ED providers and configuring the department to better accentuate family care and access.

“Themes associated with 1-star reviews among EDs and urgent care centers were similar for communication, telephone experience, billing, pain management, and diagnostic testing.”
The levers: identify the roadblocks associated with these problems and remove them; create incentives and accountability around these areas.

“Themes unique to 1-star ED reviews were service and speed of care.”
The levers: drill down further to identify the components of “service.” If possible, enlist technology to identify critical time-based milestones such as door-to-provider devise solutions, and test their efficacy.
It’s not always doing something wrong that results in a negative review; sometimes, it’s only doing the basics for your patients. Here, we examine behaviors that can impact patient perception. Consider this your prescription for 5-star service.
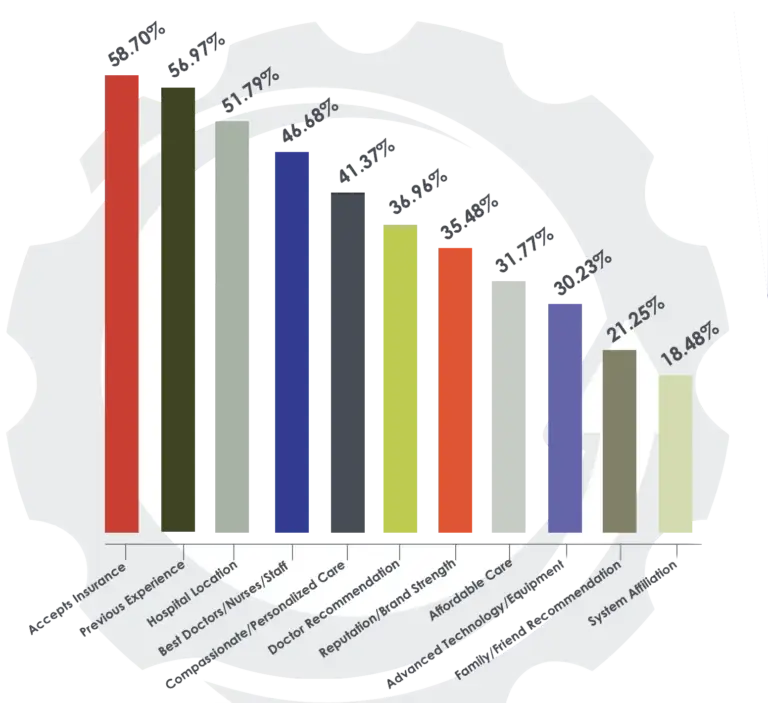
As this chart shows, some of the drivers of loyalty can only be tackled at the administrative level: which insurance the health system accepts, hospital location, and whether or not the care is “affordable” can’t be changed except at the highest decision-making level.
However, five of the top 11 drivers are directly related to patient experience.
They are more subjective (i.e., different people might define “best,” “compassionate,” and “personalized” differently) — and that means they may be influenced more readily.
Many people seem to think health systems should be looking to the digital tools and customer service practices of massive retailers like Amazon. The comparison has merits and (obvious) limitations. While making the experience of care a positive one—not least when that “customer” is afraid, or ill, or overwhelmed—is undoubtedly harder in a healthcare setting than in the typical retail scenario, some of the aspects of an excellent retail experience do carry over.
In terms of healthcare, those elements might include:
It may seem superfluous to figure out a simpler registration workflow when the stakes of other processes are so much higher. Yet this attention to the details of the visit—from the patient’s perspective—can increase patient trust, and confirm that they’ve come to the right place for care.
Different hospitals and health systems have started building more long-term trust with patients by tackling various parts of the loyalty puzzle. Some loyalty-aimed initiatives being modeled today include moving toward comprehensive price transparency; expanding access to existing patients by saving more same-day appointment slots and extending office hours; and improving care coordination, for instance by assigning navigators for oncology patients juggling services and appointments.
What changes should you prioritize for the greatest impact? Here are the ones we’ve determined to be the most effective in earning loyalty from your patients:
Of all the loyalty-oriented changes possible, this area is perhaps the most essential. This kind of anticipation can be clinical and non-clinical, but is always predicated on seeing things from the patient’s perspective. Crucially, then, it converts that empathy into action.
In the ED, this type of anticipation can take several forms:
As these examples suggest, the people patients will recognize as anticipating their needs (or not) are likely to be front-line clinicians, reception employees, and billing staff. Yet these people cannot on their own reorient work processes (like testing protocols) or set pain management policy.
Even if the push for patient commitment begins in the ED, it must be supported and reinforced across the health system. In our “Utilizing Data” section, we discuss how health systems can support front-line providers and staff who seek to anticipate patient needs—and describe what a data-driven continuous circle might look like in the ED.
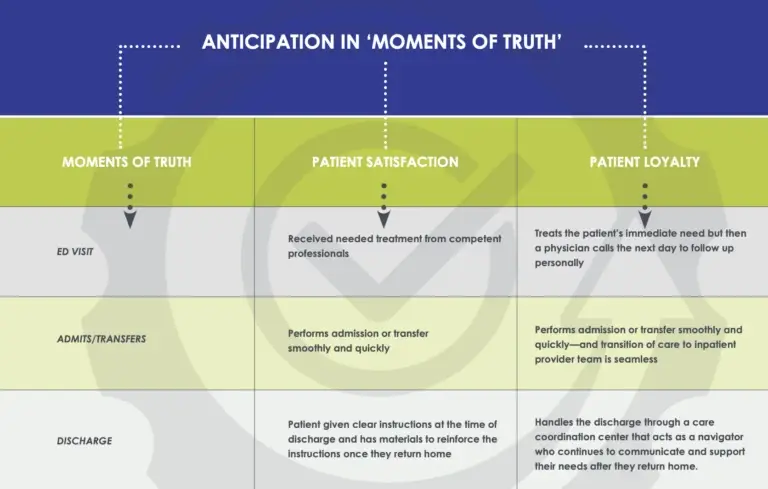
Going beyond your physical facilities is a key principle to creating loyalty. Instead of restricting care and communication to a patient’s hospital visit, that patient should understand that they have a partner they can rely on at any time. That means having access to health information and medical history records 24/7 via a robust patient portal, but it also means communication driven by the providers themselves, especially when patients feel vulnerable or passive. Having an ED physician call a patient the day after discharge is unheard of today. For that very reason, that outreach or something similar would likely feel monumental to a patient. That gap between expectation and what’s delivered feeds back into the earlier discussion of the “experience economy.” ED physicians stand to build immense trust by exceeding the current expectations that they are always on to the next patient and are too busy to follow up.
Patients today often feel bewildered by the new healthcare options that have cropped up in the past few years. The principle to keep in mind is that they’re looking for guidance, so the health system can earn trust by acting as an expert guide.
If you feel a sharp pain in your stomach, should you go to the ED? An urgent care center? Walgreens? Health systems can best help patients not by sending every person with a stomachache to the hospital, but rather by advising them to access the cheapest, quickest, and most appropriate care site. In other words, health systems should help patients navigate our fragmented healthcare system in the way that best fits the patient’s needs and means.
Before the Visit
Imagined as either a traditional call center staffed by knowledgeable, licensed nurses or as an online triage service making use of natural language recognition software and decision-making algorithms, this would serve as a resource for patients wondering whether they need to go to the ED or if another option would be better. This would be the ideal place to inform patients about non-traditional points of care, too, thus improving access and affordability.
After the Visit
This follow-up service takes different forms depending on the originating entity, but the emphasis is on keeping people well after a visit to the ED and emphasizing the primary care physician’s role in the health partnership. After a patient has been discharged and is back at home, a patient navigation representative, who is a healthcare professional, will follow up with the patient directly, to ensure they have a PCP and have scheduled a follow-up visit. If not, they can help the patient choose one or find a clinic in the community and stay on the line to help them schedule an appointment. Some patient navigation services use three-way calling to make sure the patient gets follow-up care, or they can just give the patient a referral; it depends on the patient’s needs.
So far we’ve mainly focused on two domains of change for health systems interested in moving from satisfying their patients to acquiring loyalty from their patients: anticipating needs and thinking beyond the patient’s physical visit to the health system. A third domain is utilizing data, meaning how a health system can aggregate and interpret information in order to inform behavior.
The behavior piece is critical: too often, health systems collect data only as a response to compliance requirements or other external demands. This information—whether it’s extraneous questions for the EMR, redundant insurance queries, or irrelevant satisfaction questions —is seen as an answer to someone else’s question rather than a dynamic and accessible resource for clinicians and staff. Without a sense of its utility, data collection (and data entry) can seem burdensome, sometimes even pointless.
Changing focus from satisfaction to loyalty requires a revised perspective on data use as well.
Data is often the missing link between a health system that’s interested in patient commitment and a health system that earns it. For instance, a patient might rate a clinical unit highly on a satisfaction survey but still leave the hospital feeling frustrated because the billing staff doesn’t have updated information about her account. Health systems that are serious about loyalty will invest in getting all staff the information they need to provide individualized, informed attention—no matter their department.
In education, “teaching to the test” is acknowledged as a poor substitute for thorough, student-centered instruction. It’s the same in healthcare: the outsized focus on a single episode reflects a fragmented, siloed view of patient care—a perennial flaw of our healthcare system. The shift to loyalty resets the incentives to “teach to the test” or otherwise narrow the focus from the patient’s lifetime health. It also vastly outweighs the VBP bonuses and even the HCAHPS-related reimbursement on the table—especially as patients pay an increasing share of the cost of care.
The point of a well-rounded education is a well-rounded student, one who’s engaged in learning outside the walls of the school and beyond graduation. So what does a loyal patient look like? And how does that loyalty manifest in terms of the health system’s investment?
We know how you measure patient satisfaction, but what are the right metrics for patient loyalty?

To make the switch from the left column to the right means reminding everyone in the organization, from physicians to customer service representatives, that while they may only see the patient for a small fraction of time, the sum of the patient’s experience includes all those fractions. In other words, it’s not just one friendly scheduler or the work of one skilled surgeon that defines the patient’s experience: it’s the overall culture of the organization—the ability to anticipate the needs of patients, think outside of the box, and incorporate actionable insights through data.
6 Hospital Management Strategies to Thrive in Today’s Healthcare Environment
Learn how to create patient loyalty programs and five other proven tactics for succeeding in the evolving healthcare landscape.
A W.I.S.E. Approach to Patient Satisfaction
Explore the four primary ways you can provide excellent patient experience.
5 Ways Hospital Executives Can Improve ED Patient Experience
Get best practice for improving your hospital’s ED experience and driving excellence in patient engagement.
Learn more about SCP’s programs and solutions. Talk with one of our experts today.
Sign up for our newsletter to receive the latest updates and exclusive content straight to your inbox.

A physician-led team of clinical specialists in emergency, hospital, and critical care medicine, supporting local clinical practices with national resources to deliver high-quality patient care in the communities we serve.
Corporate Phone: (800) 893-9698
Copyright © 2025. All rights reserved.
Please visit SCP Health’s Insurance Request Portal to submit requests related to medical malpractice liability insurance such as coverage verifications, claims history reports, and certificates of insurance. If you experience issues with the portal submission or have a question about the process, please reach out SCP Health’s Risk Management, Safety and Insurance Department at RM@scphealth.com or 337-609-1250.
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
Please provide your contact information. An SCP representative will contact you accordingly.