
Protecting Your Investment in Employed Physician Practices
Home » Protecting Your Investment in Employed Physician Practices
Protecting Your Investment in Employed Physician Practices
Home » Protecting Your Investment in Employed Physician Practices

Home » Protecting Your Investment in Employed Physician Practices
Home » Protecting Your Investment in Employed Physician Practices

In this white paper, we will discuss primary concerns and benefits for health systems with employed provider models, with key takeaways for hospital leaders such as:
 Introduction
IntroductionFor over 25 years, health systems have invested in employed physician practices to varying degrees. Recently, we’ve begun to see a significant shift toward this trend with the percentage of hospital-employed practices on the incline, increasing by more than 70% from 2012-2018 according to the Physician’s Advocacy Institute. Though not a brand-new phenomenon, what has changed is how these employed providers are managed in light of the healthcare industry’s stronger focus on using technology and quality metrics to achieve financial goals.
According to a recent Advisory Board survey, the top priority of hospital and health system CEOs has shifted to revenue growth and leaning on providers as a critical part of margin management initiatives. An employed provider model often costs health systems an average annual loss of $250k per employed physician. While there are very good reasons to make this investment, you need to effectively manage employed practices in order to maximize the return. According to Health Affairs, economists estimate that if health system productivity increased by 4%, the cost problem would be solved—and much of that productivity change can be driven by providers
Before starting to make any changes, it can be useful to identify the ideal profile of providers in your facility or system so the providers and hospital leadership are aligned in the goals they are pursuing and the expectations they have. While this might seem like a task for your Human Resources department, it is imperative that system leaders are invested and involved in navigating the course for such a large and influential group of employees. While the specifics will vary from one hospital or system to another, there are a few critical pieces of the ideal physician criteria that transcend factors like region, facility size, or case mix.
No matter what, you want to ensure you are hiring and cultivating providers who are:
In order to build this type of culture, hospital leaders have to appreciate how and why the trend of provider employment is developing and changing the healthcare landscape.
Leadership must tune in to why providers are interested in this model, be ready to work through the concerns they have about it, and be prepared to address both. Without first understanding the different perspectives and goals that each group brings to the table, you won’t be able to engage effectively.
In the graphic below, you’ll find the common opportunities and concerns felt by providers and health systems/ hospitals with this model. Once you get feedback from your own stakeholders, you can build out a similar chart to help organize the information and guide your next steps.
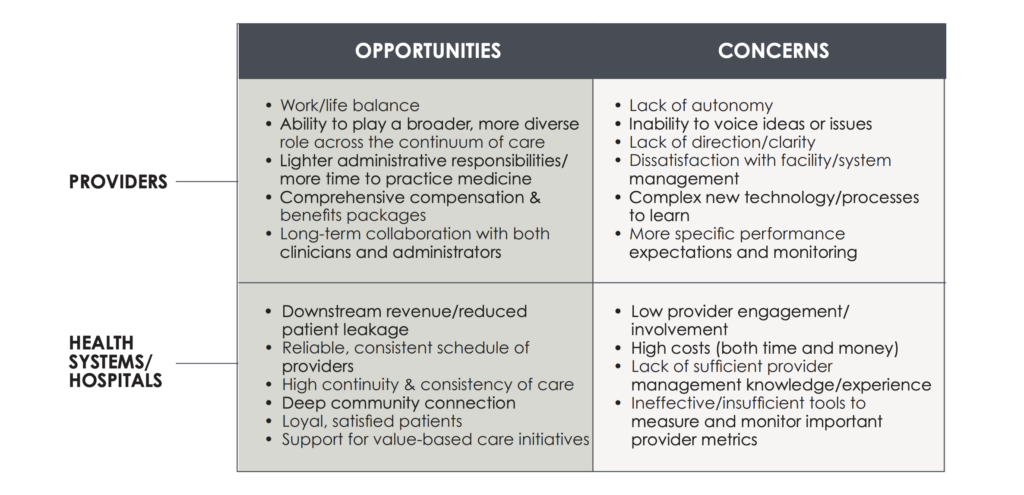
When the employment model is managed correctly, the opportunities outweigh the concerns. Providers can have more innovative, fulfilling careers while health systems and hospitals can comprehensively serve their patient communities. In order to capitalize on the benefits and solve the challenges of both health systems and providers, leaders have to move beyond just understanding – and start acting. Depending on the hospital or system, this action can be entirely driven by internal leadership or can involve direction from external practice management partners. If you find a collaborative, committed partner to work with, it can be extremely valuable to lean on the experience and objective view of an external team that specializes in provider practice management.
Regardless of what direction you take, there are three primary action areas that are imperative to building the culture you want, keeping the providers you need, and satisfying the patients you serve.
These action areas also serve as performance indicators; by measuring the impact, you can track success over time and see how you’re progressing.
The overall performance of individual providers is crucial to focus on, because providers require different types of engagement and evaluation than other clinicians and hospital employees. To manage them effectively, leaders need to:
Providers are highly talented and in high demand, so in order to maximize their value and keep them fulfilled in their work, leaders need to look closely at productivity. This includes taking steps to:
In this final action area, leaders need to zoom out from individual provider metrics and look at performance more broadly. You can slice this many ways, but we recommend working to:
Throughout these three action areas, it’s clear that establishing a management culture that enables providers to achieve high productivity and performance requires a few common threads: Effective communication, financial alignment, and necessary reporting and management tools. We call these three common threads the critical success factors—and they are your keys to optimizing your investment in employed providers.
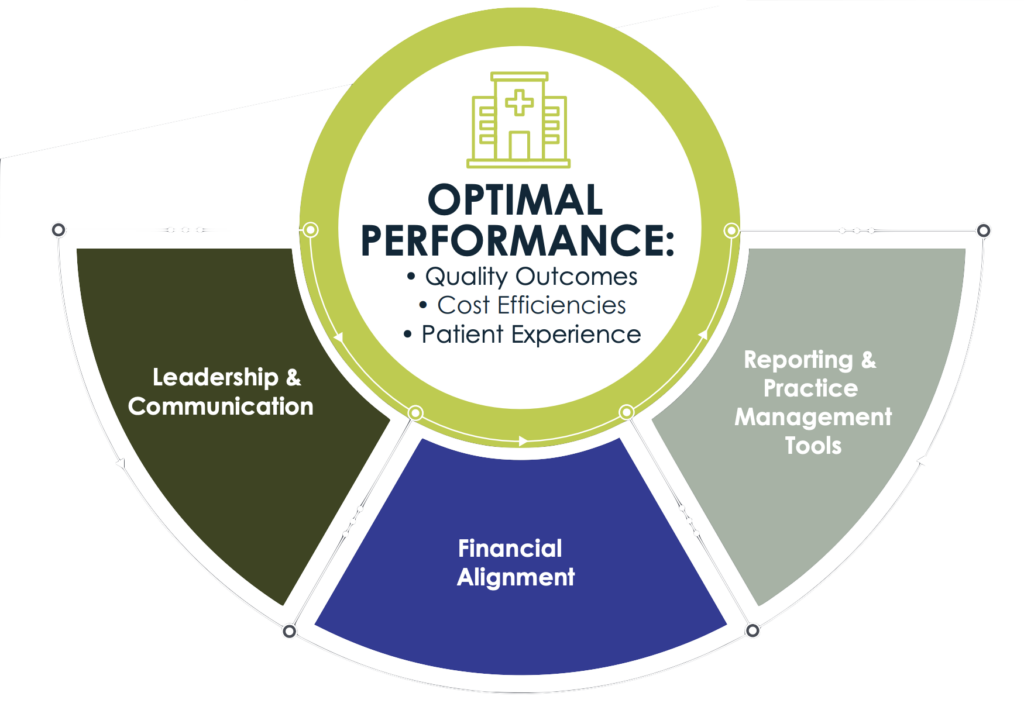
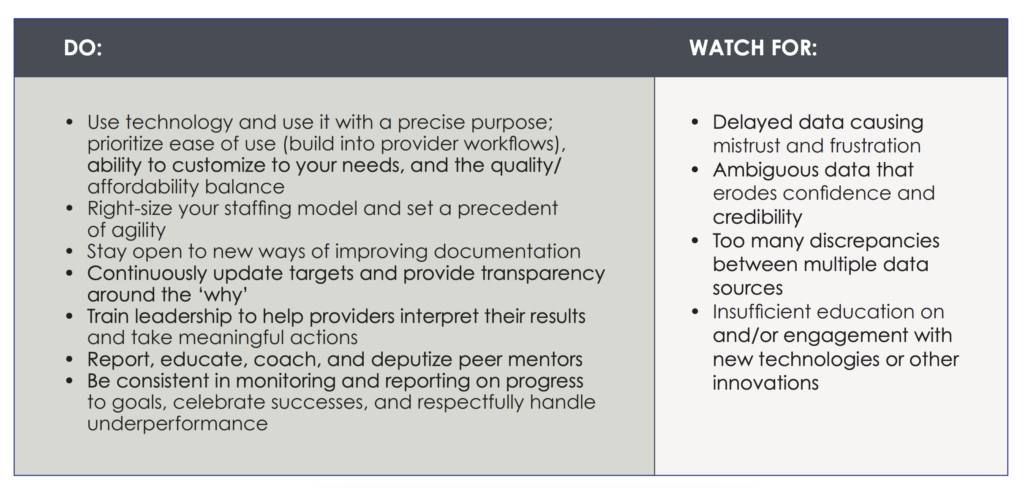
Now that you are armed with these three critical success factors, what should you do and what should you watch for to ensure optimal performance?
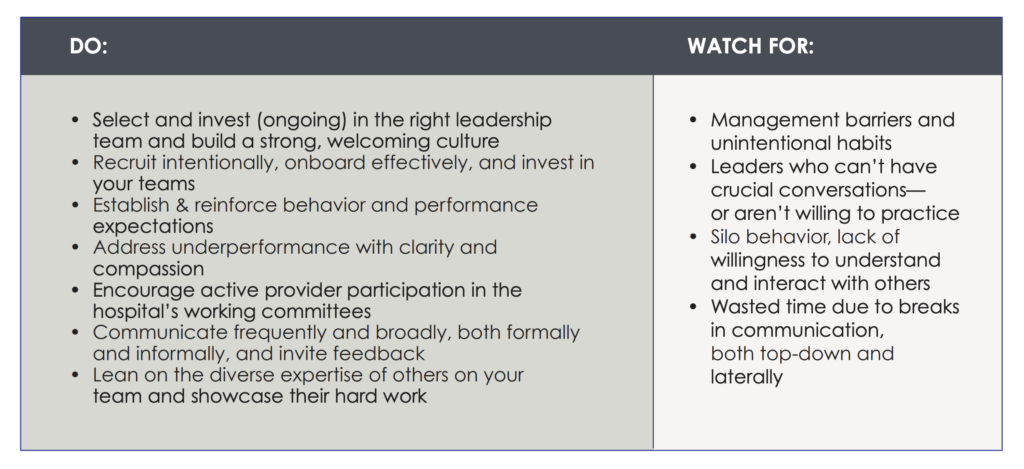
 Leadership & Communication
Leadership & CommunicationWithout communication, you can’t have strong leadership; without leadership, communication will be ineffective and underwhelming.
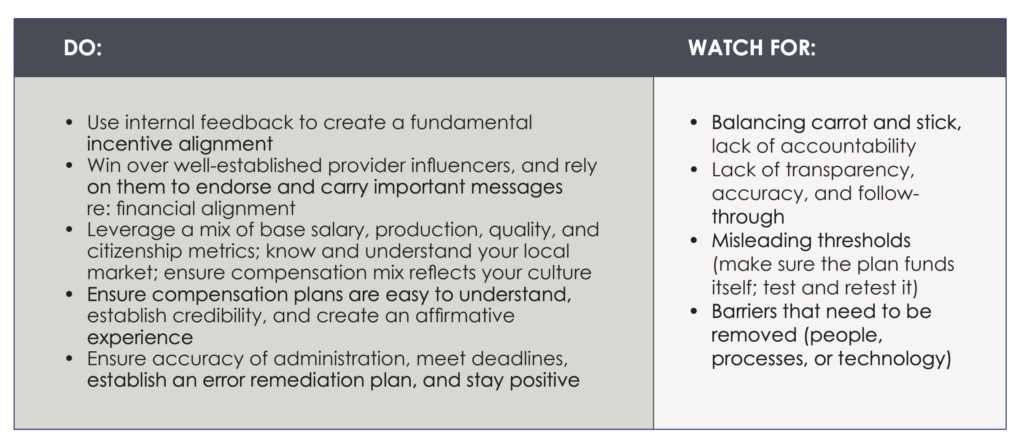
 Financial Alignment
Financial AlignmentGetting everyone on the same financial page may sound like an intimidating task, but it’s likely more manageable than you think—and it’s an undeniable necessity.
 Reporting and Practice Management Tools
Reporting and Practice Management ToolsLaunching strategic initiatives and embracing innovations is fantastic—but if you can’t measure progress or impact, you’ll just be spinning your wheels.
If you’re preparing to employ your own providers or planning to improve your existing employed model, you might be asking yourself how best to implement this information and get started. As mentioned earlier, leaders can work to optimize their provider management strategy internally or can choose to lean on an external practice management partner for guidance and relief—either for bits and pieces of the process or as a comprehensive solution. When navigating this decision, leaders should consider the following factors as they relate to both options:
Regardless of what approach you choose, one thing is certain: you have to be aligned. According to Health Catalyst, a major reason that many change management or performance improvement efforts fail is that multiple people are working on random pieces of the same initiative without an overarching plan or interactive communication. If you are going to create and sustain a high-performing, successful employed provider model, you have to take inventory of all current related projects, assess their efficacy, and make a clear plan to move forward. All key stakeholders must be invested in that plan and ready to do what it takes to execute it. If your people are disconnected, your efforts are disjointed, or your decisions are disagreed upon, your chances of success will surely suffer.
Once that general plan of action is agreed upon by all your key stakeholders, you can begin working through those question exercises of “which management strategies can we implement to influence provider productivity and performance?” and “how can we weave the critical success factors into everything we do?” Together, your team (no matter who it’s comprised of) can work through the answers, deploy the tactics you feel are right for your organization, continuously monitor progress, and make changes to your plan accordingly.
While the decision to keep management efforts internal or involve external experts is something each leadership team has to decide on its own, the following case study briefly demonstrates how using an external practice management partner helped Centura Health enhance and optimize its investment in employed providers.
After a period of massive growth, Centura Health, a 17-hospital system, was looking for support as it developed its 10- year strategic plan. In order to achieve their aspirational goals, system leaders needed to first create a unified culture that would effectively represent and support its diverse group of physicians. The system optimized its investment in employed providers by partnering with SCP Health to establish a strong, collaborative, physician-empowering practice management program within the Centura Health Physician Group. The system’s overarching goals, SCP Health’s primary strategies, and the remarkable quantifiable impact of the partnership are displayed in the graphic below.
Not for profit, faith-based, 17 facilities, 6,000+ physicians, employed hospital medicine group
 In Summary
In SummaryTo summarize what we’ve covered throughout this paper, let’s review where we’ve been in 8 simple takeaways:
Case Study: Revenue Cycle and Documentation Assurance Management Partnership Produce Measurable Results
Case Study: Enhancing Program Economics and Building a Culture of Continuous Improvement
Blog: Improving the Performance of Employed Providers
Blog series:
Guide: A Game Plan for Recruiting the Right (& Retainable) Provider
Want to learn more about how we can take your hospital performance to the next level? Contact us today.
Sign up for our newsletter to receive the latest updates and exclusive content straight to your inbox.

A physician-led team of clinical specialists in emergency, hospital, and critical care medicine, supporting local clinical practices with national resources to deliver high-quality patient care in the communities we serve.
Corporate Phone: (800) 893-9698
Copyright © 2025. All rights reserved.
Please visit SCP Health’s Insurance Request Portal to submit requests related to medical malpractice liability insurance such as coverage verifications, claims history reports, and certificates of insurance. If you experience issues with the portal submission or have a question about the process, please reach out SCP Health’s Risk Management, Safety and Insurance Department at RM@scphealth.com or 337-609-1250.
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
By clicking the “Submit” button, you are agreeing to the SCP Heath Terms of Use and Privacy Policy
Please provide your contact information. An SCP representative will contact you accordingly.